by Duaa Eldeib
This story was originally published by ProPublica. ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Stillbirths
When Babies Die Before Taking Their First Breath
Lying on her living room sofa, her head cradled just under her husband’s shoulder, Brooke Smith pulled out a pen and began marking up her medical records.
Paging through the documents, she read a narrative that did not match her experience, one in which she said doctors failed to heed her concerns and nurses misrepresented what she told them. In anticipation of giving birth to her first child in the spring of 2014, Brooke had twice gone to the hospital in the weeks leading up to her due date because she hadn’t felt the baby kick, her medical records show. And twice doctors had sent her back home.
Brooke, a Black singer-songwriter who has worked as a New York City elementary school teaching assistant, has kept her medical records as a reminder of all that unfolded and all that she believes could have been prevented.
After that second hospital admission, and following some testing, she was diagnosed with “false labor” and discharged, records show, though she was 39 weeks and 3 days pregnant and insisted that her baby’s movements had slowed. Research shows that after 28 weeks, changes in fetal movement, including decreased activity or bursts of excessive fetal activity, are associated with an increased risk of stillbirth. The risk of delivering a stillborn child also continues to rise at or after 40 weeks.
Six days later, she and her husband, Colin, met friends for breakfast. Brooke, then 33, had pancakes with whipped cream, the kind of sugary meal that usually prompted kicks from her baby within minutes. When the baby didn’t move, she told her husband they needed to return to the hospital for a third time.
Her due date had come and gone; this time she wasn’t leaving until doctors delivered her baby.
But at the hospital they learned their baby, a girl they had named Kennedy Grey, had died in Brooke’s womb. She would have to deliver their stillborn daughter.
The doctor, the same one who had been on call during her second hospital admission less than a week before, asked her when she last felt the baby move. Brooke said she had felt rapid, almost violent kicking two days earlier, followed by wave-like movements. The doctor, Brooke said, told her that she should have come in earlier.
“If they would have listened to me earlier, I would have delivered a living baby,” Brooke said recently. “But if you’re a Black woman, you get dismissed because it’s like, ‘What are you complaining about now?’”
For Brooke, her experiences in the last weeks of her pregnancy, along with what she later discovered in her medical records, crystallized what researchers and medical experts have found: While many pregnant people say their doctors and nurses do not listen to them and their concerns are often dismissed, pregnant Black people face an even higher burden.
One 2019 study that looked at people’s experience during their pregnancy and childbirth lamented the “disturbing” number of patients who reported a health care provider ignored them, refused their request for help or failed to respond to such requests in a reasonable amount of time. The study found pregnant people of color were more than twice as likely as white people to report such “mistreatment.”
Another study looking at stillbirths that occurred later in pregnancy highlighted the “importance of listening to mothers’ concerns and symptoms,” including “a maternal gut instinct that something was wrong.”
Every year more than 20,000 pregnancies in the U.S. end in stillbirth, the death of an expected child at 20 weeks or more. But not all stillbirths are inevitable. This year, ProPublica has reported on the U.S. stillbirth crisis, including the botched rollout of the COVID-19 vaccines for pregnant people, the proliferation of misinformation, the failure to do enough to lower a stubbornly high national stillbirth rate and the lack of study of the causes of stillbirths.
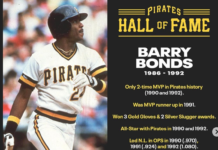
Data from the federal Centers for Disease Control and Prevention tells the story of how the U.S. health care system has failed Black mothers in particular. Black women overall are more than twice as likely as white women to have a stillbirth, according to 2020 CDC data, the most recent available. In some states, including South Carolina, Kansas and Tennessee, they are around three times as likely to deliver a stillborn baby.
In Arkansas and Mississippi, the stillbirth rate for Black women in 2020 topped 15 per 1,000 live births and fetal deaths; it was more than 11 in New Jersey and New York. The national stillbirth rate for Black women was 10.3 and for white women 4.7.
But drawing focus to Black stillbirths is a challenge in a country where stillbirths, in general, have been understudied, underfunded and received little public attention. In addition, the community of stillbirth researchers and advocates remains relatively small and overwhelmingly white.
Academic studies and national obstetric groups have explicitly identified racism as one of the factors that contribute to persistent health disparities. In 2020, in the wake of the pandemic and the murder of George Floyd at the hands of police, the American College of Obstetricians and Gynecologists joined around two dozen obstetric and gynecologic health organizations to issue a statement expressing their commitment to “eliminating racism and racial inequities” that lead to disparities.
“Systemic and institutional racism are pervasive in our country and in our country’s health care institutions, including the fields of obstetrics and gynecology,” the statement reads.
Nneka Hall, a maternal health advocate and doula trainer who recently served on Massachusetts’ Special Commission on Racial Inequities in Maternal Health, said disparities are embedded in the health care system, including unequal rates of stillbirths and dying during pregnancy or soon after.
Black women face nearly three times the risk of maternal mortality than white women, according to CDC data. Even at higher educational levels, Black people die during pregnancy or childbirth at higher rates than their white counterparts, as do their babies. Pregnant people are also more likely to deliver prematurely if they are Black.
“It’s the Black experience,” said Hall, whose daughter Annaya was stillborn. “You’re told that you have to advocate for yourself, but when you’re in a melanated body and you advocate for yourself, it’s not taken seriously. If you raise your voice, you’re being abusive or abrasive. If you say you know something, you’re automatically shown that you don’t know as much as you think you know.”
For years, Dr. Ashanda Saint Jean has heard the stories of Black patients who, before they suffered the devastating loss of delivering a stillborn baby, said they tried to tell their doctors and nurses that something was wrong.
But they said they were dismissed by their medical team. Even shut down.
With each new story, Saint Jean asked the same question: Would they have been treated differently if they had not been Black? Far too often, she concluded, the answer was yes.
“Those are the stories I hear that break my heart,” she said.
Saint Jean, chair of the obstetrics and gynecology department at Health Alliance Hospitals of the Hudson Valley, said those patients, the very same ones who face an increased risk of stillbirth, are left feeling powerless.
“We know that this is certainly a public health crisis, and it should be a public health priority,” said Saint Jean, a diversity, equity and inclusive excellence adviser for ACOG and associate professor of obstetrics and gynecology at New York Medical College.
The risk of a stillbirth increases along with the number of “significant life events” a pregnant person faces, including job loss, an inability to pay bills or the hospitalization of a close family member. Black people who are pregnant, research shows, are more likely than their white counterparts to report multiple stressful life incidents.
In 2020, a CDC report examining racial and ethnic disparities in stillbirths identified several factors that might be at play, including the patient’s health before pregnancy, socioeconomic status and access to quality health care, as well as stress, institutional bias and racism. The report found the “disparities suggest opportunities for prevention to reduce” the stillbirth rate.
A spokesperson for ACOG said that the group has been working for years to eliminate racial inequities through policy, training, guidance and advocacy. The group has publicly acknowledged the field’s disturbing history, including the fact that James Marion Sims, who’s known as the “father of gynecology,” conducted medical experiments on enslaved Black women.
Last year, the CDC launched a racism and health web portal, and CDC director Dr. Rochelle Walensky declared racism a serious public health threat, saying in a statement that racism isn’t just discrimination but “the structural barriers” that influence how people live and work.
Dr. Terri Major-Kincade, a neonatologist and health equity expert in Texas, said it’s misguided to highlight disparities among different racial groups without recognizing the lingering effects of racism. She said racism, not race, is responsible for the disparities.
One recent modeling analysis funded by the National Institutes of Health determined lowered levels of segregation decreased the odds of stillbirth for Black people, but had no effect on stillbirths for white people. The researchers estimated decreasing segregation could prevent about 900 stillbirths a year for expectant Black parents.
“A dedicated provider is not going to outshine a system that’s compromised by years of structural bias,” Major-Kincade said. “The system is going to win every time.”
The first and easiest step, she said, is listening to pregnant Black women.
“We can’t prevent every stillbirth,” she said, “but we can sure prevent a lot if we listen.”
Eight years after her daughter was stillborn, Brooke still has days she can’t get out of bed. She replays in her mind how she begged her medical team to listen to her concerns about the baby’s lack of movement as she neared her due date. After nurses hooked her up to a monitor and the baby moved, someone on the staff told her that children often make “liars” out of their parents. Another time, Brooke said, they told her the baby was being “lazy.”
She witnessed the same mindset reflected in her medical records. She studied each line carefully, scribbling comments in the margins. When she reached the notes from her hospital admissions, she gasped and turned to her husband. “Can you believe this?” she asked him. A nurse had written that Brooke “reports she is very bad at monitoring and feeling” fetal movement, the records show.
“I never said I was bad at monitoring,” Brooke wrote at the time. “I mentioned that she doesn’t move the way they say she should.”
As a Black woman, Brooke knew all too well that racial disparities existed. She and her friends had traded stories of their own inequities and indignities. And she had felt the sting of doctors questioning her pain and office employees asking if she would be able to pay her medical bills.
When Brooke learned she was pregnant, she thought she could find a way around those disparities by going to what she called a hospital where women from the country club went. For each appointment, she drove nearly an hour each way from her home in Queens to Long Island Jewish Medical Center.
Back at home, she and Colin prepared for their daughter’s birth. They liked the name Kennedy Grey because it was unique and gender-neutral. In her nursery, they assembled her crib and picked out a bright pink sheet to match the pink letters of her name on her toy box. Brooke, who grew up in Brooklyn and planned to pass down her impeccable style to her daughter, filled a closet with billowy tulle dresses, cozy footed pajamas and tiny Converse infant booties.
And so, when they arrived at the hospital that final time and the doctor told them she couldn’t find Kennedy’s heartbeat, Brooke told her to check again. And again.
“We were in shock,” she said. “We didn’t scream. We didn’t cry. We didn’t believe it.”
Three separate ultrasounds did not detect a heartbeat, but Brooke and Colin held steadfast to their Christian faith. The doctor wrote in the medical records that Brooke and her family believed that “the fetus may be born alive and will require resuscitation.” Just maybe, Brooke recalled thinking, Kennedy’s heart rate was too faint for the machines to pick up.
After more than 12 hours of labor, Brooke delivered her daughter. When Kennedy was placed in her arms, Brooke gave her mouth-to-mouth. For years to come, she thought to herself, she would tell the story of how the doctor had said her baby was dead, but she was mistaken, and then Brooke would point to her beautiful daughter beside her.
An autopsy would later find signs in the baby’s lungs of deep gasps before she died, and her umbilical cord, which had a knot in it, was wrapped around her neck. The sudden burst of movement Brooke felt before her daughter died, research suggests, may have been a fetal seizure caused by the lack of oxygen.
“There’s a lot of self-blame and guilt,” said Brooke, her gentle brown eyes overshadowed by her dark-rimmed glasses. “Why didn’t I fight more? Why didn’t I say more? And then I try to come to a level of peace and say, ‘You trusted your medical providers.’ When we get medical care, that’s exactly what we’re doing. We’re putting our lives in these people’s hands.”
The Smiths sued the medical staff, the hospital and the hospital system, Northwell Health, making many of the allegations about her care. The medical providers denied wrongdoing. The lawsuit was dismissed after Brooke, who by then had a young son at home and was looking for new attorneys after her old ones withdrew from the case, missed a court date.
In response to questions from ProPublica, a spokesperson for Northwell Health did not answer questions about Brooke’s care. The spokesperson extended the hospital system’s sympathies to Brooke and her family, adding, “We understand our responsibility to our patients who entrust their care with us.
“Northwell Health strives to provide the best possible care for each individual patient,” said the spokesperson. “At Northwell, we have ongoing performance improvement processes to continually evaluate our guidelines and treatments with the goal to provide optimal care for birthing people and their babies.”
Women of color have been fueling a growing underground movement creating maternal health programs that focus on equity and reproductive justice.
Kanika Harris is the director of maternal and child health at Black Women’s Health Imperative, a long-standing national nonprofit organization created for and by Black women focusing specifically on the health and wellness of Black women and girls.
For years, Harris said, Black women were grateful to have been invited to discuss their ideas and explain the trauma they faced to researchers, health care leaders and government officials, but little changed. Building their own organizations not only fills a void left by the groups that have not met the needs of people of color, it also signals a commitment to celebrate and learn from a rich history of traditional and supportive practices in their communities.
Harris is separately working with another organization to establish a birth center in Detroit, which they say would become the first Black-led birth center in Michigan.
“We can’t wait for hospitals to figure it out,” said Harris, who lives in Washington, D.C. “We have to do this ourselves. My daughter can’t go through what I went through.”
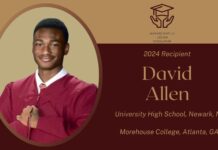
In 2010, Harris delivered twins, a boy named Kodjo, who was stillborn, and a girl named Zindzi, who died a few days later. Both the fetal death report and the death certificate list Harris’ race as Black and her education as “8th grade or less.” At the time, Harris was preparing her doctoral dissertation in health behavior and health education from the University of Michigan.
Sitting in the car after meeting with the pathologist who walked through Kennedy’s autopsy results, Brooke and Colin Smith decided to launch a nonprofit to raise awareness about stillbirth and help families who had experienced pregnancy or infant loss. A key part of empowering families, Brooke said, is educating them about stillbirths.
Like many parents, she and Colin didn’t know stillbirths still happened.
They both decided to go back to school to get bachelor’s degrees in social work, and they are now pursuing master’s degrees so they can continue supporting families.
Brooke’s grief has intensified as the years have passed, building from an initial shock to a feeling that rarely leaves her. It has taken her time to figure out how to resume the ordinary rhythms of life and navigate being around other children whose mothers were pregnant at the same time as her. She went to one child’s birthday party, but hasn’t been able to bring herself to attend others. On her and Colin’s wedding anniversary, they got matching “K” tattoos on their ring fingers.
In 2018, Eric Adams, then Brooklyn borough president and now mayor of New York City, officially commended the Smiths for their nonprofit work and proclaimed May 19 as Kennedy Grey Community Service Day.
As gratifying as the recognition is, she can’t help but feel disheartened that after years of advocacy to reduce stillbirths, substantial reform has yet to be achieved. It’s not enough to extend condolences for her loss, Brooke said. She wants change.
Sometimes she lies awake at night thinking about the few hours she was able to spend with Kennedy. She and Colin took pictures of their daughter, one of which is still the lock screen image on her phone. The nurses wrapped her in the leopard-print blanket they brought to take her home in and slipped her feet into her pink Converse booties. Brooke and Colin asked their family to film them with their daughter.
“It’s May 19, and this is our dear Ms. Kennedy Grey. We just wanted to have a video with our daughter,” an exhausted Brooke said into the camera. She sang a song she had composed for her. As her melodious voice carried through the room, Colin reached over and stroked Kennedy’s cheek. When it was his turn, he recited the nursery rhyme “This Little Piggy” as he squeezed Kennedy’s toes.
Brooke hadn’t shed a single tear in the hospital, not until the end, when she could no longer deny that her daughter had died. A nurse entered the room to take Kennedy away. She clutched Kennedy tighter.
“Don’t take my baby,” she wailed. “Don’t take my baby.”
It was the last time she would see her daughter.
Image: Camylla Battani/Unsplash