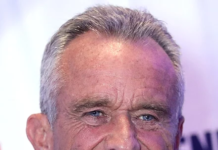
BYLINE: Kristina Sauerwein/
Newswise — New findings on long COVID — long-term effects on health experienced by many who have had COVID-19 — present a good-news, bad-news situation, according to a study at Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care system.
The bad news: COVID-19 patients who were hospitalized within the first 30 days after infection face a 29% higher risk of death in the third year compared with people who have not had the virus. However, the three-year death risk still marks a significant decline compared with such risk at the one- and two-year marks post-infection. The findings also show that even people with mild COVID-19 were still experiencing new health problems related to the infection three years later.
The good news: The increased risk of death diminishes significantly one year after a SARS-CoV-2 infection among people who were not hospitalized for the virus. This demographic accounts for most people who have had COVID-19.
The new research, published May 30 in Nature Medicine, tracked the virus’s health effects in people three years after being infected with the original strain of COVID-19 in 2020. That year, about 20 million people tested positive for the virus in the U.S. The new study assessed the risk of death and 80 adverse health conditions in people three years after being diagnosed with COVID-19.
“We aren’t sure why the virus’s effects linger for so long,” said senior author Ziyad Al-Aly, MD, a Washington University clinical epidemiologist and a global leader in long COVID research. “Possibly it has to do with viral persistence, chronic inflammation, immune dysfunction or all the above. We tend to think of infections as mostly short-term illnesses with health effects that manifest around the time of infection. Our data challenges this notion. I feel COVID-19 continues to teach us — and this is an important new lesson — that a brief, seemingly innocuous or benign encounter with the virus can still lead to health problems years later.”
Up to 10% of people infected with the virus experience long COVID, according to federal data.
Al-Aly’s prior research has documented COVID-19’s damage to nearly every human organ, contributing to diseases and conditions affecting the lungs, heart, brain, and the body’s blood, musculoskeletal and gastrointestinal (GI) systems.
Such studies with longer follow-up are limited, said Al-Aly, a nephrologist who treats patients at the Washington University-affiliated John J. Cochran Veterans Hospital in midtown St. Louis. “Addressing this knowledge gap is critical to enhance our understanding of long COVID and will help inform care for people suffering from long COVID.”
Al-Aly and his team analyzed millions of de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated health-care system. The study included more than 114,000 veterans with mild COVID-19 who did not require hospitalization; more than 20,000 hospitalized COVID-19 patients; and 5.2 million veterans with no COVID-19 diagnosis. Patients were enrolled in the study from March 1, 2020, to Dec. 31, 2020, and followed for at least three years, until Dec. 31, 2023. Patients included people of diverse ages, races and sexes; statistical modeling ensured parity in representation.
In the third year after infection, COVID-19 patients who had been hospitalized experienced a 34% elevated health risk across all organ systems compared with people who did not have COVID. That number is down from a 182% increased risk one year after a COVID infection and a 57% risk two years after.
Among nonhospitalized patients, researchers found a 5% increased risk in suffering from long COVID in the third year after infection. This translates into 41 more health problems per 1,000 persons – a small but not trivial burden. The long-term health effects in the third year primarily affected the GI, pulmonary and neurological systems. By comparison, the risk was increased by 23% one year after infection and increased by 16% two years after.
In the analysis, researchers also measured and compared the number of healthy life-years lost due to COVID-19. They found that among the nonhospitalized, at three years after infection, COVID-19 had contributed to 10 lost years of healthy life per 1,000 persons. By comparison, three years post-infection, those hospitalized for COVID-19 had experienced 90 lost years of healthy life per 1,000 persons.
For context, in the U.S., heart disease and cancer each cause about 50 lost years of healthy life per 1,000 persons, while stroke contributes to 10 lost years of healthy life per 1,000 persons.
“That a mild SARS-CoV-2 infection can lead to new health problems three years down the road is a sobering finding,” said Al-Aly, who is also director of the Clinical Epidemiology Center at the VA St. Louis Health Care System, and head of the research and development service. “The problem is even worse for people with severe SARS-CoV-2 infection. It is very concerning that the burden of disease among hospitalized individuals is astronomically higher.”
“COVID-19 is a serious threat to the long-term health and well-being of people and it should not be trivialized,” he said.
The extended trajectory for long COVID may change as researchers incorporate data from years beyond 2020. At that time, vaccines and antivirals had not been developed. Similarly, Al-Aly’s analysis does not consider subsequent variants such as omicron or delta.
“Even three years out, you might have forgotten about COVID-19, but COVID hasn’t forgotten about you,” Al-Aly said. “People might think they’re out of the woods, because they had the virus and did not experience health problems. But three years after infection, the virus could still be wreaking havoc and causing disease or illness in the gut, lungs or brain.”
Image: kjpargeter/freepik