Background
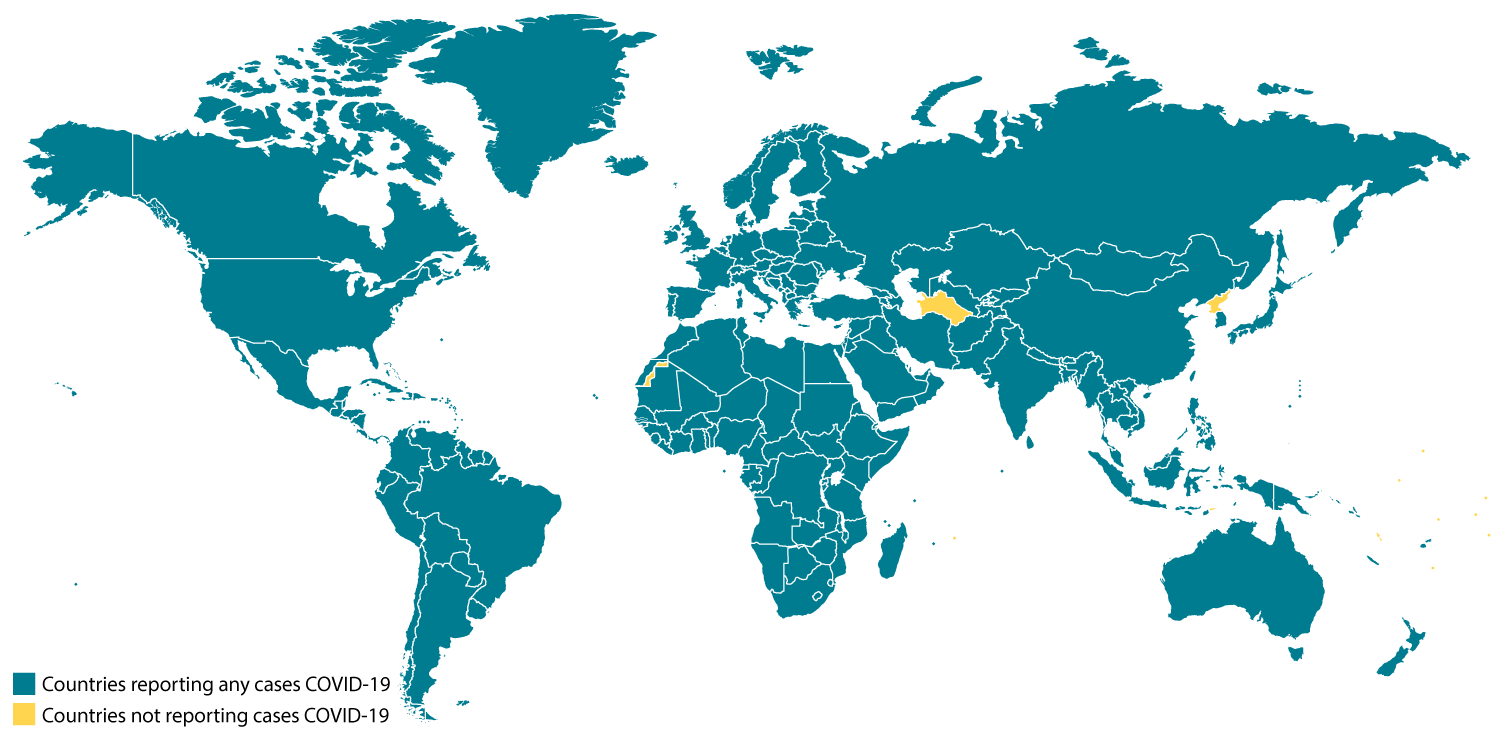
CDC is responding to an outbreak of respiratory disease caused by a novel (new) coronavirus that was first detected in China and which has now been detected in more than 100 locations internationally, including in the United States. The virus has been named “SARS-CoV-2” and the disease it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”).
On January 30, 2020, the International Health Regulations Emergency Committee of the World Health Organization declared the outbreak a “public health emergency of international concernexternal icon” (PHEIC). On January 31, 2020, Health and Human Services Secretary Alex M. Azar II declared a public health emergency (PHE) for the United States to aid the nation’s healthcare community in responding to COVID-19. On March 11, 2020 WHO publiclyexternal icon characterized COVID-19 as a pandemic.
Source and Spread of the Virus
Coronaviruses are a large family of viruses that are common in people and many different species of animals, including camels, cattle, cats, and bats. Rarely, animal coronaviruses can infect people and then spread between people such as with MERS-CoV, SARS-CoV, and now with this new virus (named SARS-CoV-2).
The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats. The sequences from U.S. patients are similar to the one that China initially posted, suggesting a likely single, recent emergence of this virus from an animal reservoir.
Early on, many of the patients at the epicenter of the outbreak in Wuhan, Hubei Province, China had some link to a large seafood and live animal market, suggesting animal-to-person spread. Later, a growing number of patients reportedly did not have exposure to animal markets, indicating person-to-person spread. Person-to-person spread was subsequently reported outside Hubei and in countries outside China, including in the United States. Some international destinations now have apparent community spread with the virus that causes COVID-19, as do some parts of the United States. Community spread means some people have been infected and it is not known how or where they became exposed. Learn what is known about the spread of this newly emerged coronaviruses.
Situation in U.S.
- In addition to CDC, many public health laboratories are now testing for the virus that causes COVID-19. View CDC’s Public Health Laboratory Testing map.
- With this increase in testing, more and more states are reporting cases of COVID-19 to CDC. View latest case counts, deaths, and a map of states with reported cases.
- U.S. COVID-19 cases include:
- Imported cases in travelers
- Cases among close contacts of a known case
- Community-acquired cases where the source of the infection is unknown.
Illness Severity
The complete clinical picture with regard to COVID-19 is not fully known. Reported illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death. While information so far suggests that most COVID-19 illness is mild, a reportexternal icon out of China suggests serious illness occurs in 16% of cases. Older people and people of all ages with severe underlying health conditions — like heart disease, lung disease and diabetes, for example — seem to be at higher risk of developing serious COVID-19 illness.
Learn more about the symptoms associated with COVID-19.
There are ongoing investigations to learn more. This is a rapidly evolving situation and information will be updated as it becomes available.
Risk Assessment
Outbreaks of novel virus infections among people are always of public health concern. The risk to the general public from these outbreaks depends on characteristics of the virus, including how well it spreads between people; the severity of resulting illness; and the medical or other measures available to control the impact of the virus (for example, vaccines or medications that can treat the illness). That this disease has caused severe illness, including illness resulting in death is concerning, especially since it has also shown sustained person-to-person spread in several places. These factors meet two of the criteria of a pandemic. As community spread is detected in more and more countries, the world moves closer toward meeting the third criteria, worldwide spread of the new virus.
It is important to note that current circumstances suggest it is likely that this virus will cause a pandemic. This is a rapidly evolving situation and CDC’s risk assessment will be updated as needed.
Current risk assessment:
- For the majority of people, the immediate risk of being exposed to the virus that causes COVID-19 is thought to be low. There is not widespread circulation in most communities in the United States.
- People in places where ongoing community spread of the virus that causes COVID-19 has been reported are at elevated risk of exposure, with increase in risk dependent on the location.
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also are at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring also are at elevated risk of exposure, with increase in risk dependent on location.
CDC has developed guidance to help in the risk assessment and management of people with potential exposures to COVID-19.
What May Happen
More cases of COVID-19 are likely to be identified in the United States in the coming days, including more instances of community spread. It’s likely that at some point, widespread transmission of COVID-19 in the United States will occur. Widespread transmission of COVID-19 would translate into large numbers of people needing medical care at the same time. Schools, childcare centers, and workplaces, may experience more absenteeism. Mass gatherings may be sparsely attended or postponed. Public health and healthcare systems may become overloaded, with elevated rates of hospitalizations and deaths. Other critical infrastructure, such as law enforcement, emergency medical services, and sectors of the transportation industry may also be affected. Healthcare providers and hospitals may be overwhelmed. At this time, there is no vaccine to protect against COVID-19 and no medications approved to treat it. Nonpharmaceutical interventions would be the most important response strategy.
CDC Response
Global efforts at this time are focused concurrently on lessening the spread and impact of this virus. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this public health threat.
CDC is implementing its pandemic preparedness and response plans, working on multiple fronts, including providing specific guidance on measures to prepare communities to respond to local spread of the virus that causes COVID-19. There is an abundance of pandemic guidance developed in anticipation of an influenza pandemic that is being adapted for a potential COVID-19 pandemic.
Highlights of CDC’s Response
- CDC established a COVID-19 Incident Management System on January 7, 2020. On January 21, CDC activated its Emergency Operations Center to better provide ongoing support to the COVID-19 response.
- The U.S. government has taken unprecedented steps with respect to travel in response to the growing public health threat posed by this new coronavirus:
- Foreign nationals who have been in China or Iran within the past 14 days cannot enter the United States.
- U.S. citizens, residents, and their immediate family members who have been in China or Iran within in the past 14 days can enter the United States, but they are subject to health monitoring and possible quarantine for up to 14 days.
- On March 8, CDC recommended that people at higher risk of serious COVID-19 illness avoid cruise travel and non-essential air travel.
- Additionally, CDC has issued the following additional specific travel guidance related to COVID-19.
- CDC has issued clinical guidance, including:
- On January 30, CDC published guidance for healthcare professionals on the clinical care of COVID-19 patients.
- On February 3, CDC posted guidance for assessing the potential risk for various exposures to COVID-19 and managing those people appropriately.
- On February 27, CDC updated its criteria to guide evaluation of persons under investigation for COVID-19.
- On March 8, CDC issued a Health Alert Network (HAN).
- CDC has deployed multidisciplinary teams to support state health departments case identification, contact tracing, clinical management, and public communications.
- CDC has worked with federal partners to support the safe return of Americans overseas who have been affected by COVID-19.

This is a picture of CDC’s laboratory test kit for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). CDC tests are provided to U.S. state and local public health laboratories, Department of Defense (DOD) laboratories and select international laboratories.
- An important part of CDC’s role during a public health emergency is to develop a test for the pathogen and equip state and local public health labs with testing capacity.
- CDC developed an rRT-PCR test to diagnose COVID-19.
- As of the evening of March 8, 78 state and local public health labs in 50 states and the District of Columbia have successfully verified and are currently using COVID-19 diagnostic tests.
- Combined with other reagents that CDC has procured, there are enough testing kits to test more than 75,000 people.
- In addition, CDC has two laboratories conducting testing for the virus that causes COVID-19. CDC can test approximately 350 specimens per day.
- Commercial labs are working to develop their own tests that hopefully will be available soon. This will allow a greater number of tests to happen close to where potential cases are.
- CDC has grown the COVID-19 virus in cell culture, which is necessary for further studies, including for additional genetic characterization. The cell-grown virus was sent to NIH’s BEI Resources Repositoryexternal icon for use by the broad scientific community.
- CDC also is developing a serology test for COVID-19.
CDC Recommends
- Everyone can do their part to help us respond to this emerging public health threat:
- Individuals and communities should familiarize themselves with recommendations to protect themselves and their communities from getting and spreading respiratory illnesses like COVID-19.
- Older people and people with severe chronic conditions should take special precautions because they are at higher risk of developing serious COVID-19 illness.
- If you are a healthcare provider, be on the look-out for:
- People who recently traveled from China or another affected area and who have symptoms associated with COVID-19, and
- People who have been in close contact with someone with COVID-19 or patients with pneumonia of unknown cause. (Consult the most recent definition for patients under investigation [PUIs].)
- If you are a healthcare provider or a public health responder caring for a COVID-19 patient, please take care of yourself and follow recommended infection control procedures.
- If you are a close contact of someone with COVID-19 and develop symptoms of COVID-19, call your healthcare provider and tell them about your symptoms and your exposure. They will decide whether you need to be tested, but keep in mind that there is no treatment for COVID-19 and people who are mildly ill are able to isolate at home.
- If you are a resident in a community where there is ongoing spread of COVID-19 and you develop COVID-19 symptoms, call your healthcare provider and tell them about your symptoms. They will decide whether you need to be tested, but keep in mind that there is no treatment for COVID-19 and people who are mildly ill are able to isolate at home.
- For people who are ill with COVID-19, but are not sick enough to be hospitalized, please follow CDC guidance on how to reduce the risk of spreading your illness to others. People who are mildly ill with COVID-19 are able to isolate at home during their illness.
- If you have been in China or another affected area or have been exposed to someone sick with COVID-19 in the last 14 days, you will face some limitations on your movement and activity. Please follow instructions during this time. Your cooperation is integral to the ongoing public health response to try to slow spread of this virus.
Other Available Resources
The following resources are available with information on COVID-19
Story Credits To: